IT STARTED with “CSI.” The photogenic medical examiners are scouring a dead victim’s body for clues and the cameras gratuitously zoom in on the gory details. Ever since, graphic autopsies have popped up on seemingly every police procedural and detective drama on television.
But have you ever wondered what happens in a real autopsy, the kind that occurs every day in hospitals all around the world? Everybody dies. Sometimes someone wants to know why.
After shifting careers following more than a decade in journalism, I’m a first-year pathology resident at a Chicago-area hospital. This year, I’ve gotten a crash course in autopsies. Follow me to the morgue, if you dare.
But, before we begin, a warning: if you’re eating your lunch now, it might be best to read something else.
Still with me? Here we go.
Morgues usually are in the hospital basement, the bowels of the building, so to speak, in an area that most visitors never see. No one wants a grim reminder that some admissions end up here. The morgue includes a walk-in refrigerator where the recently departed lie on carts in body bags awaiting their next move to a funeral home or an autopsy.
The autopsy occurs in a room with long metal tables attached to large sinks. There are aging anatomy posters on tile walls with institutional colors like tan or lime-green. On the shelves, buckets contain brains soaking in formalin, a formaldehyde preservative solution, which combines with the other pungent ambient smells of bleach and disinfectants.
The first (living) people we encounter are the “dieners,” the term for the autopsy assistants, who open up the body and make the organs accessible for examination.
It’s not a job for everyone, but the dieners have done this hundreds, if not thousands of times, on bodies of every shape and size. They have crazy stories. They do a lot of the dirty work, from eviscerating to, in some cases, using ladles to scoop out and measure bloody fluid that can accumulate inside body spaces of the very ill. Six liters of reddish liquid straight out of the abdomen in one case I saw.
See? I warned you.
The other people here are doctors, more specifically pathologists. Most pathologists spend the bulk of their time peering through microscopes at tumors and biopsies to determine whether the cells they’re seeing are cancerous or some other diseased state. But they also are responsible for autopsies.
At academic hospitals, that means pathology residents. Dissecting cadavers, of course, is a rite of passage for all medical students, an intense lesson in anatomy and the finality of death that can be harrowing, humbling and fascinating. But as a pathology resident, this is no one-off experience. Pathology residents are required to perform 50 autopsies during their four years of residency. Every path resident is acutely aware of how many he or she has done. I’ve done nine now. Eighteen percent of the way there.
Every time the dieners unzip that body bag, I’m hit with a wave of anxiety. “Am I really going to do this?”
It’s a strange place to find one’s self after a liberal arts education and years of making a living in news. The decision to go to med school in my late 30s was a complicated one, spurred by turmoil in the newspaper business and a lifetime of interest in the sciences, which, as a journalist, I had written about often.
In college biology, I had enjoyed looking through microscopes at amoebas and dissecting frogs, so pathology drew my attention as the most scientific of the medical fields. Pathology means “the study of disease,” a rich area to explore and a potential source for future writing.
Still, it’s a long way from the lively bustle of the newsroom to a second career that includes scrutinizing the dead.
In the news business, you are no stranger to tragedy. As a reporter, I’d written plenty of obituaries. I’d covered deadly car crashes, fatal fires, shocking homicides and destructive tornadoes. But interviewing subjects and writing words is very different from holding, in your hands, the heart of a patient who had died just hours earlier.
You do get used to it once you’ve done it a few times though. Kind of.
~
In the past, autopsies were more frequent. Pathology residents commonly performed a hundred or more. Nationwide autopsy rates on hospital deaths declined from 41 percent in 1964 to about 15 percent in 1983, according to the American Medical Association. By 2007, the percentage dropped to 8.5 percent, according to the Centers for Disease Control’s NationalCenter for Health Statistics.
The reasons are many. Advancements in diagnostic technology such as computed tomography (CT) and magnetic resonance imaging (MRI) have taken a lot of mystery out of why someone dies. Also, with people living longer, more deaths are occurring at long-term care facilities and hospice settings. Furthermore, hospitals generally do not charge families for autopsy services and insurers do not usually pay for autopsy costs, so that makes autopsies a “loss leader” which hospitals must manage. Nowadays, the reason a family may request an autopsy for a loved one is to see if they have grounds for a malpractice suit.
But autopsies are important not just for bewildered family members trying to understand a cause of death. Examining the body post-mortem provides pathologists-in-training with intimate experience with organs and diseases that they will encounter throughout their careers. The autopsy report also yields valuable information for the physicians who had been involved in the patient’s care in their dying days which may help guide them as they face similar decisions with future patients.
~
Before beginning the autopsy, we review the patient’s medical history. In pathology, we don’t see the patient before they die. We are with them at a moment after the drama of their last breath and before the wakes and funerals, when tearful loved ones say their final goodbyes. The only insight we get into the patient’s personal life is the name of the person who signed the consent form for the autopsy, usually a spouse or child. Where was the patient born? Did she have grandchildren? What did she do for a living? Did she play piano or tennis? We don’t know these things, and maybe it’s for the best.
It’s time to get dressed. We start in hospital scrubs. Over that, we slip on a disposable plastic gown with long sleeves. We wear shoe covers and a hospital hair net. We put on a mask with a see-through panel that covers our eyes because, yes, something could splash into our eyes. We wear rubber gloves: usually three layers of them, but sometimes as many as six if the patient has an infectious disease such as hepatitis or HIV.
In our textbooks, there are photos of physicians a century ago performing autopsies with their bare hands. Gross anatomy.
After the dieners wheel the body into the room and double-check its identity, we start the external exam. Basically, we look over the corpse and write down what we see.
I’d prefer to avoid looking at the pale, lifeless faces of the autopsy patients, but there’s no way around it. We measure the pupils and document the condition of the eyes. We examine the patient’s teeth. We document nasogastric tubes in the nostrils or endotracheal tubes in the mouths of patients who had trouble breathing near the end.
These faces have appeared in my recent dreams.
Then, we describe the degree of rigor mortis and livor mortis — which is the way gravity pulls blood to the lower parts of a body after death, causing the skin to appear purplish-red. We measure scars. We notice burn marks left on the chest from resuscitation attempts after cardiac arrest. We press the skin on the shins to check for swelling. If the toenails have a fungal infection, we write it down.
~
The internal exam is when it really gets grisly. The dieners make a Y-shaped incision over the patient’s chest. They use an electric bone saw to slice open the sternum. The buzz lets us know the innards are coming soon.
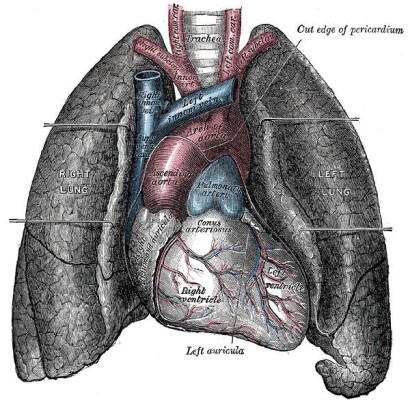
The lungs and heart arrive first. When you hold a healthy lung, it has a crackly feeling of countless tiny air-filled alveoli, like microscopic packing bubbles. When lungs are filled with fluid they feel solid, almost the consistency of liver, and that might mean pneumonia.
We use sharp scissors to cut open vessels and bronchi to look for clots or mucus plugs that may have impaired breathing. Then we make slices into the lungs with a 10-inch razor at every half-inch or so, a process pathologists call “bread-loafing.” The idea is to look for tumors, areas of infarction or other signs of disease that might be hiding deep in the tissue. Then we use a scalpel to slice a sample about the size of a postage stamp and plop it into a container that later will be embedded in wax, thinly sliced and applied to a glass slide that pathologists examine under a microscope.
The heart is especially tricky. We make tiny slices along the outer surface, known as the epicardium, to find the three major coronary arteries. The heart pumps blood throughout the rest of the body, but it is a muscle that needs its own blood supply. A heart attack occurs when there is a block in one of those crucial three arteries—the left anterior descending artery (aka “The Widow Maker,” because a clot here is so devastating), the left circumflex artery and the right coronary artery—so we look to see if they are clogged.
We weigh the heart. A heavy heart is bad, and not just metaphorically speaking. We also bread-loaf it. We look at the muscle walls of the ventricles to see if they are thinned out, a sign of heart failure, or thickened, often a result of chronic high blood pressure, or if they have areas lighter in color that may indicate a heart attack has occurred.
It continues with all the organs in the torso, from the thumb-sized adrenal glands to the football-sized liver. Pathologists have given many pathological conditions they encounter names based on foods they supposedly resemble. So you get terms like “nutmeg liver,” “chocolate cyst,” “bread and butter pericarditis,” “strawberry hemangioma,” and “watermelon stomach.”
I would not be the first person to observe that pathologists are a little odd.
The analogy to food is disturbing and unavoidable. We’re essentially using razors and glorified meat cleavers to slice up the organs on cutting boards. It’s best not to dwell on this. I just focus on the task at hand and re-enter the land of the living as fast as I can.
~
So what’s the most gruesome portion of the autopsy? The “running of the bowels” is a leading contender. The average human intestines are almost thirty feet long. The diener piles the floppy pink entrails into a large metal bowl, brings them to the sink and makes a slice down their entire length, opening them up and emptying the contents down the drain. The stench, as you can imagine, is formidable. The pathologist sifts through the bowel inch by inch, looking for tumors, polyps or areas of necrosis.
Removing the brain is also unforgettable. The dieners make a circular incision around the crown of the head and peel the skin over to expose the skull. It is, to me, the single most twisted and macabre scene in an autopsy. The loosely detached skin reminds me of Michelangelo’s “Last Judgment” in the Sistine Chapel, where St. Bartholomew holds the floppy, flayed skin from his horrifying martyrdom.
The dieners then use the bone saw to cut a circle out of the skull and remove it like a cap. The brain is scooped out, weighed and dropped into a bucket of formalin. After pickling for 10 days, it is stiff and well-preserved so that it too can be bread-loafed and searched for signs of strokes, tumors and infections.
~
When the autopsy is over, the dieners sew up the head. They take what remains of the organs and stash them back into the torso and sew that up too. Despite all they’ve been through, the bodies are presentable enough for an open casket.
Unlike in the television autopsies, there often is not an “A-ha” moment where you find a clear-cut cause of death. More often, a combination of factors pile up—say, heart failure, pneumonia, renal failure and sepsis—but there’s no telling what dealt the death blow.
The autopsy itself usually takes about two to four hours, but the work afterwards, including microscopic analysis of the samples we took, can stretch for weeks until an autopsy report is finalized. By that time, the body will be six feet under, as we all will be some day.
But not me. At least, not now. I’ve survived another autopsy.
Ten down, 40 to go.


Dear Mr. Biemer,
I read your article with interest, as I am a practicing Forensic Pathologist. It is discouraging that your experience with autopsies seems so negative, and leads me to wonder how exactly your introduction to postmortem examinations came about. I assure you that for those who actually practice forensic pathology, it is a field we are passionate and excited to be a part of. Not to mention that we are doing work that many others cannot stomach (as your article suggests).
I am hoping you revisit your feelings about Autopsy Pathology after you have had adequate exposure to a true forensic pathology practice. There are many great opportunities to do so and several wonderful mentors in and around the Chicago area–reach out to them during your residency training! And that “Aha!” moment you think does not exist at an autopsy? It is a part of my life each and every single day; determining why an otherwise healthy seeming person died is a sizable chunk of my job description.
I can certainly understand why the dissection is “gross” to most. But for those of us with a true love of anatomy, performing autopsies is a privilege that very few will ever be able to experience. These decedents are indeed my patients, and I hold them in the highest regard. The autopsy will be the last medical procedure they will ever experience. To me, the morgue becomes a celebration of life, and a reflection on how incredible the human body is. I am so sorry that you are incapable of seeing it this way; it feels a bit like you are wasting a precious gift.
Finally, forensic pathologists are indeed are very different from the television shows that showcase our field…namely because we are real. Please contact me if you would like to discuss this further.
Best,
Mindy Hull, MD
HullPath Forensics, LLC
mindy@hullpath.com
Dr. Hull,
Thank you for your feedback and your interest. I have nothing but respect for people like you who conduct autopsies on a regular basis. It is very important and fascinating work and I’m honored to be a part of it.
My piece was mainly targeted at a non-medical readership, explaining what happens in a real medical autopsy and what that experience is like for someone who is just learning to do it. And clearly my experience is shaped by the fact I am, as of now, still coming to terms with the very human emotions that are stirred up by it.
Thanks again,
John Biemer, MD
Thank you for the article. I considered medical school for quite awhile while working at the career I retired from, that of being a police officer in Richardson, Texas. Had I done so, my interest would have been forensic pathology because of witnessing my first autopsy in 1976 at the Dallas County Institute of Forensic Sciences which was being performed by Charles Petty, MD. who was wearing his trademark bow tie, a plastic dishwasher’s apron and kitchen rubber gloves.
One of the things that first intrigued me was to learn that the bodies were stored in a walk-in cooler as you describe, however, they were not covered with anyone other than whatever was on them when they arrived. The explanation was that any cover could lead to the loss of trace evidence on the outside of the body from friction or condensation. Altogether, it and the other autopsies I’ve witnessed through work were endlessly fascinating.
Pingback: Mindy Hull, MD
Hey John:
I read your piece with interest, and it made me vividly recall my first day of respiratory-care clinicals at Edward Hospital in Naperville. After decades in journalism, I, like you, found myself in scrubs, facing the unknown in what Shakespeare called ”the undiscovered country.” I was about two months shy of my 50th birthday, standing alongside someone on whose high school diploma the ink was barely dry. I was flat-out scared, asking myself as you did, am I really here, can I really do this? I checked the vitals and Spo2 of my 92-year-old patient, shocked by her nakedness and how little attention anyone else in the room paid to it. I fought back the waves of nausea, reminding myself that I was going on a journey that would test not only my intellect, but also my physical fortitude. But at that moment, I was losing. As the attending physician asked me to remove the patient’s false teeth, and her daughter began wailing for us to save her mother’s life, I doubted my resolve. But after stabilizing the patient and cleaning her blood from my shoes after drawing my first ABG, I thought that maybe I could do this. And I did.
Your essay was dead-on accurate. I learned more than I ever thought possible in two years, and discovered parts of myself I didn’t know were in there. My only regret was not taking that odyssey when I was about 22. Still, I’m happy to report that I graduated with top honors and was hired at Good Samaritan Hospital in Downers Grove. After than a year, I was recruited by Newsday, and taken a hiatus from respiratory care and returned to the newsroom on Long Island.
To keep my feet wet in the field, I do per diem work with my RRT brother. And while I don’t miss the long shifts in the ICU and the ER, I do miss my patients and camaraderie of my team, several of whom I went through the program at the College of DuPage. And, like you, I’ve proved to myself that it’s never too late to chase a dream, even those that seem uncatchable. Take care of yourself and your patients.
Always the best,
Jeffrey L. Williams
RRT for life
Whatever the case, cost should never be weighed against what you intend to benefit in the long run. For instance, a school nurse
gets a fixed salary with small yearly increases, but gets excellent benefits from the state or county that includes
a generous vacation package and retirement plan. Observing the overall health of the client including their
social and emotional well being in there home.